Blue Cross Blue Shield Federal Employee Program Standard Vs Basic
Blue Cross Blue Shield Federal Employees Program and Blue Cross Blue Shield Florida covers weight loss surgery.
ObesityCoverage strongly feels that morbid obesity is a disease and every insurance company should cover these life saving procedures. So we are happy to report that BCBS Florida and BCBS Federal covers weight loss surgery. In fact, most of the Blue Cross Blue Shield network has some sort of coverage for weight loss surgery.
It is important to know that your employer can typically opt-out of weight loss surgery insurance coverage for their employees policies. This typically saves the company money on their premiums. Contact information for BCBS Federal and BCBS Florida is listed below.
Even if your policy excludes weight loss surgery, because BCBS has shown that these types of surgeries are medically necessary you might be able to appeal their exclusion. Before calling make sure you see our questions to ask before calling your insurance company section.
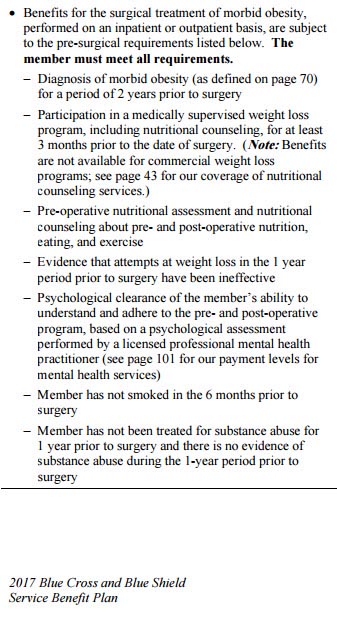
BCBS Federal Employees Program Pre-Approval Requirements
The items below are the minimum necessary for approval of your weight loss surgery.
- Body Mass Index of 40 or greater OR BMI 35 or more with comorbidities.
- Documentation of failed diets by conservative treatment.
- Letter of support from primary care physician.
- 18 years of age.
- Gastric bypass and Lap-band procedures are covered. Gastric Sleeve is usually covered as well.
BCBS Florida Pre-Approval Requirements
- BMI of 35 or greater
- Diagnosed as morbidly obese for at least 5 years
- Documentation of physician supervised non-surgical management weight loss program (e.g., diet, exercise, drugs) for at least 6 consecutive months
- No thyroid or endocrine disorders
- Psychological evaluation
- Letter from PCP supporting the medical necessity of weight loss surgery
- Gastric bypass, Lap-band and BPD/DS procedures are covered. Sleeve gastrectomy may be covered.
- Revisions: covered for one of the following conditions and/or diagnoses:
- weight loss of 20% or more below the ideal body weight,
- esophagitis, hemorrhage or hematoma complicating a procedure,
- vomiting following gastrointestinal surgery,
- gastrointestinal complications (i.e., complications of intestinal anastomosis and bypass),
- stomal dilatation (documented by endoscopy not UGI),
- pouch dilation documented by upper gastrointestinal examination or endoscopy producing weight gain of 20% or more,
- stomal stenosis after vertical banding documented by endoscopy and producing vomiting or weight loss of 20% or more,
- other and unspecified post surgical non-absorption, other postoperative functional disorders,
- severe dumping syndrome,
- post-gastric surgery syndromes,
- disruption of operation wound,
- staple line failure documented by upper gastrointestinal examination,
- disrupted staple line provided there has been prior weight loss
From page 70 in their manual:
Types of Weight Loss Surgeries Covered By BCBS FEP and BCBS Florida
Recently gastric sleeves have begun to be covered by some of the large insurance companies as a primary weight loss surgery. Currently, gastric sleeves are typically covered by both of these policies.
Covered Weight Loss Surgery Procedures
- Laparoscopic Gastric Bypass
- Gastric Sleeve
- Open Gastric Bypass Surgery
- Gastric Banding – including the Lap Band and Realize Band
- Duodenal Switch also known as Biliopancreatic Diversion
Lap Band Fills Covered?
BCBS considers Lap Band Fills a Medical Necessity when required to meet the proper level of weight loss. This is true only if you've had a previous adjustable gastric banding procedure that met all of the criteria laid out for that procedure. Typically, if you paid cash for the procedure ongoing lap band fills will not be covered by insurance.
Is a Second Weight Loss Surgery Covered if Gastric Banding Didn't Work?
Surgical procedures following a previous weight loss surgery that did not result adequate weight loss, such as a lap band or realize band to a gastric bypass, gastric sleeve or duodenal switch are covered by insurance when the following criteria are met:
- The patient continues to meet all the medical necessity criteria for bariatric surgery, and
- There must be documentation that the patient was compliant with the original post-operative dietary and exercise program, and
- 2 years after the original weight loss surgery, weight loss is still less than 50% of pre-operative excess body weight and weight remains at least 30% of the patients ideal body weight, per BMI.
Revisions
Revisions are covered if there is documentation of a failure secondary to a surgical complication. Complications can include but are not limited to fistula, obstruction or disruption of a suture/staple line.
Does BCBS Federal and BCBS Florida Require Surgery at a Center Of Excellence?
Yes, weight loss surgery must be done at a Center of Excellence. These are referred to as Blue Distinction Centers and can be found on the BCBS website.
BCBS FEP and BCBS Florida's Contact Info to Inquire About Surgery
BCBS Federal Employees Program can be found here.
BCBS Florida's contact information can be found here.
Source: https://www.obesitycoverage.com/bcbs-federal-employee-program-and-florida-blue-weight-loss-surgery-requirements/
0 Response to "Blue Cross Blue Shield Federal Employee Program Standard Vs Basic"
Post a Comment